A Urinary Tract Infection (UTI) is a common and often painful infection that affects any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. While UTIs can affect anyone, they are significantly more common in women. These infections occur when bacteria, usually from the skin or rectum, enter the urethra and travel up into the urinary tract. The consequences range from mild discomfort to serious health complications if left untreated, making early detection and effective management crucial. Understanding the nuances of a urinary tract infection (UTI) is the first step toward effective prevention and treatment.
This comprehensive guide delves deep into the world of Urinary Tract Infection (UTI), exploring its various forms, the underlying causes, common symptoms, diagnostic methods, and a wide array of treatment options. We’ll also cover crucial preventive measures, address specific populations at higher risk, and debunk common myths. Our aim is to equip you with the knowledge needed to recognize, manage, and ideally, prevent these often-distressing infections, ensuring better urinary health and overall well-being. Whether you’re experiencing your first UTI or dealing with recurrent episodes, this article provides authoritative, evidence-based information to help you navigate this common health challenge.
Table of Contents
What is a Urinary Tract Infection (UTI)?
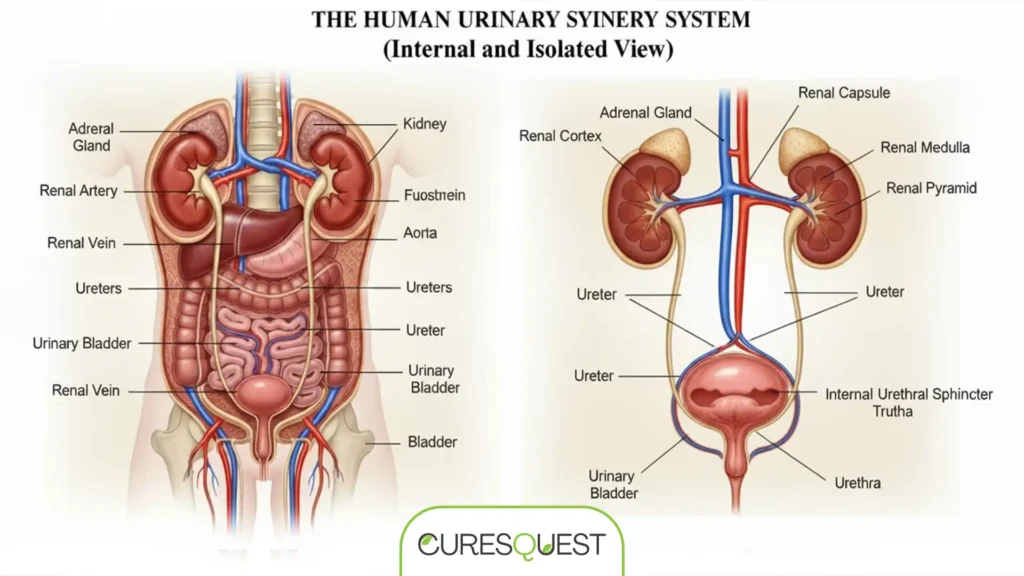
The urinary tract is a complex system designed to produce, store, and eliminate urine from the body. It consists of the kidneys, which filter waste from the blood to produce urine; the ureters, tubes that carry urine from the kidneys to the bladder; the bladder, a muscular sac that stores urine; and the urethra, a tube that carries urine from the bladder out of the body. A Urinary Tract Infection (UTI) occurs when microorganisms, most commonly bacteria, invade and multiply in any part of this system. While any part of the urinary tract can be infected, the most common type of UTI involves the lower urinary tract – the bladder and urethra.
Types of Urinary Tract Infections
UTIs are typically classified based on the part of the urinary tract they affect. Each type presents with distinct symptoms and potential severity:
- Cystitis (Bladder Infection): This is the most common type of UTI. It occurs when bacteria multiply in the bladder, leading to inflammation. Symptoms often include frequent and painful urination, a strong urge to urinate, and sometimes blood in the urine.
- Urethritis (Urethra Infection): An infection limited to the urethra, the tube that carries urine out of the body. Urethritis can be caused by bacteria that spread from the rectum or sexually transmitted infections (STIs). Symptoms include a burning sensation during urination and discharge.
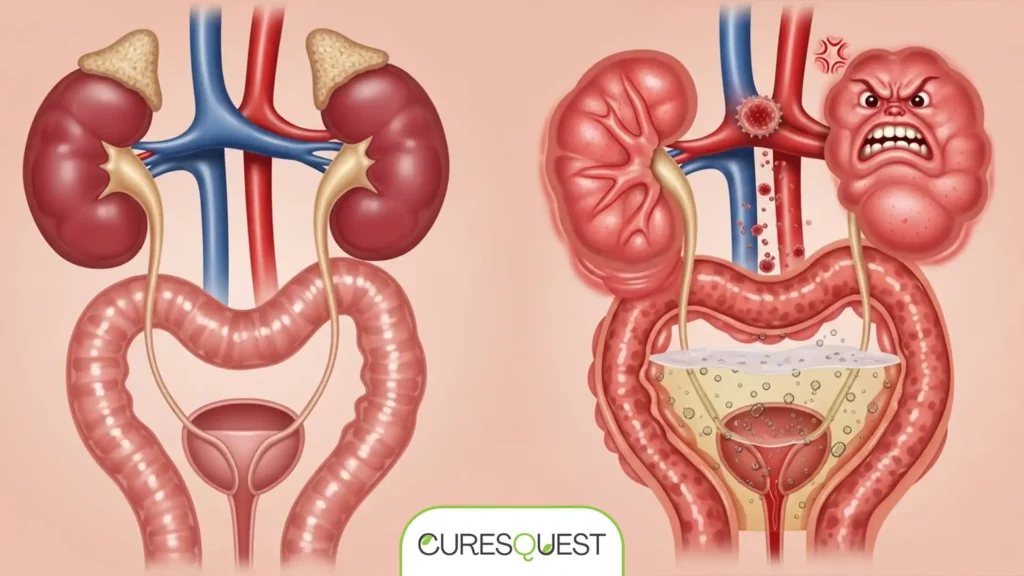
- Pyelonephritis (Kidney Infection): This is a more serious type of UTI that occurs when bacteria travel up from the bladder to one or both kidneys. Kidney infections can cause severe symptoms like high fever, chills, back or flank pain, nausea, and vomiting. If not treated promptly, pyelonephritis can lead to kidney damage or even sepsis, a life-threatening complication.
Understanding these distinctions is vital for proper diagnosis and treatment, as kidney infections require more aggressive medical intervention compared to lower urinary tract infections. Recognizing the early signs of a more severe infection can significantly impact outcomes.
Common Causes of Urinary Tract Infection (UTI)
The primary cause of a Urinary Tract Infection (UTI) is the entry of bacteria into the urinary tract through the urethra. The vast majority of UTIs are caused by Escherichia coli (E. coli), a type of bacteria commonly found in the gastrointestinal tract. However, other bacteria and, less commonly, fungi or viruses can also cause UTIs. The anatomical structure of the urinary tract, particularly in women, makes it more susceptible to bacterial invasion.
Bacterial Entry and Spread
- Anatomy: Women have a shorter urethra than men, and its opening is closer to the anus, making it easier for bacteria from the bowel to reach the bladder.
- Sexual Activity: Sexual intercourse can introduce bacteria into the urethra.
- Poor Hygiene: Improper wiping after bowel movements (wiping back to front) can transfer bacteria.
Risk Factors for Urinary Tract Infection (UTI)
Several factors can increase an individual’s susceptibility to developing a UTI:
- Gender: Women are far more prone to UTIs due to their anatomy.
- Sexual Activity: Frequent or intense sexual activity can increase risk, especially with new partners or certain types of contraception (e.g., diaphragms, spermicides).
- Menopause: Decreased estrogen levels after menopause lead to changes in the urinary tract that make women more vulnerable to infection.
- Urinary Tract Abnormalities: Birth defects or structural problems in the urinary tract can impede urine flow, creating a breeding ground for bacteria.
- Blockages in the Urinary Tract: Kidney stones, an enlarged prostate in men, or other obstructions can trap urine and increase infection risk.
- Suppressed Immune System: Conditions like diabetes or other diseases that weaken the immune system can make the body less able to fight off infections.
- Catheter Use: Individuals who use catheters to urinate are at a higher risk of developing UTIs.
- Recent Urinary Procedure: Medical procedures involving instruments inserted into the urinary tract can increase risk.
- Spermicides: Some studies suggest that spermicides can alter vaginal flora, making women more susceptible to UTIs.
Understanding these risk factors can help individuals take proactive steps to reduce their chances of developing a Urinary Tract Infection (UTI). For further reading on the causes and symptoms, you can refer to the Mayo Clinic’s detailed page on Urinary Tract Infection.

Recognizing the Symptoms of Urinary Tract Infection (UTI)
The symptoms of a Urinary Tract Infection (UTI) can vary depending on the severity of the infection, the part of the urinary tract affected, and the individual’s age and overall health. It’s crucial to recognize these signs early to seek prompt medical attention and prevent the infection from spreading or worsening. While some symptoms are common across all types of UTIs, others are more indicative of a specific location of infection.
Common Symptoms of Lower UTIs (Bladder and Urethra)
- Persistent, Strong Urge to Urinate: Feeling like you need to urinate frequently, even shortly after emptying your bladder.
- Burning Sensation During Urination (Dysuria): This is one of the most classic and uncomfortable symptoms.
- Passing Frequent, Small Amounts of Urine: Despite the strong urge, only a small amount of urine may be passed each time.
- Cloudy Urine: Urine may appear cloudy or murky due to the presence of pus or bacteria.
- Red, Bright Pink, or Cola-Colored Urine: This indicates the presence of blood in the urine (hematuria).
- Strong-Smelling Urine: Urine may have an unusually pungent or foul odor.
- Pelvic Pain: Women may experience pelvic pain, especially in the center of the pelvis and around the area of the pubic bone.
- Rectal Pain: Men may experience rectal pain.
Symptoms of Upper UTIs (Kidneys – Pyelonephritis)
Kidney infections are more severe and can lead to serious complications if not treated immediately. Symptoms often include:
- High Fever: Often accompanied by chills and shivering.
- Nausea and Vomiting: Feeling sick to your stomach and throwing up.
- Back or Flank Pain: Pain in the back, side, or groin, typically on one side, below the ribs.
- Fatigue and General Malaise: Feeling very tired and unwell.
UTI Symptoms in Specific Populations
Symptoms can be atypical in certain groups:
- Children: Young children might not articulate their symptoms clearly. Look for unexplained fever, irritability, poor feeding, vomiting, or new-onset bedwetting or accidents.
- Elderly Individuals: Older adults may not experience typical UTI symptoms like burning or frequent urination. Instead, they might exhibit confusion, agitation, falls, dizziness, or other changes in mental status, alongside general weakness or fatigue.
- Pregnant Women: UTIs are common during pregnancy and can lead to complications if untreated. Symptoms might be subtle, making regular screening important.
If you suspect you have a Urinary Tract Infection (UTI), especially if you experience symptoms of a kidney infection, it’s vital to seek medical attention promptly. Early diagnosis and treatment are key to preventing the infection from worsening and causing more significant health issues. For additional information on recognizing symptoms, Harvard Health offers a comprehensive A-to-Z guide on Urinary Tract Infection.
Diagnosing a Urinary Tract Infection (UTI)
Accurate diagnosis is the cornerstone of effective treatment for a Urinary Tract Infection (UTI). When you visit a healthcare provider with suspected UTI symptoms, they will typically perform a physical examination and order specific tests to confirm the diagnosis, identify the type of bacteria, and determine the most effective course of treatment.
Medical History and Physical Exam
Your doctor will start by asking about your symptoms, medical history, and any risk factors you may have. A physical examination may also be performed, which could include checking for tenderness in your abdomen or flank area.
Key Diagnostic Tests
- Urinalysis: This is the most common initial test. You’ll be asked to provide a clean-catch urine sample. The sample is then analyzed for the presence of white blood cells, red blood cells, and bacteria, which are indicators of infection. Nitrites and leukocyte esterase, produced by bacteria and white blood cells respectively, are also key markers.
- Urine Culture: If a urinalysis suggests an infection, a urine culture is usually performed. This test involves growing bacteria from your urine sample in a lab to identify the specific type of bacteria causing the infection. It also helps determine which antibiotics will be most effective against that particular strain (antibiotic sensitivity testing). This is crucial for guiding targeted treatment and preventing antibiotic resistance.
- Imaging Tests: For recurrent UTIs or if a kidney infection is suspected, your doctor might order imaging tests to look for abnormalities in your urinary tract. These can include:
- Ultrasound: Uses sound waves to create images of the kidneys and bladder.
- CT Scan: Provides more detailed cross-sectional images of the urinary tract.
- MRI: Another advanced imaging technique.
- Cystoscopy: In some cases, a thin, flexible tube with a camera (cystoscope) may be inserted into the urethra to view the bladder and urethra directly. This is usually reserved for complex or recurrent cases.
It’s important to provide a clean-catch urine sample to avoid contamination, which can lead to inaccurate results. Your healthcare provider will give you instructions on how to collect the sample correctly. Prompt and accurate diagnosis ensures that you receive the right treatment quickly, preventing the infection from progressing and reducing the risk of complications.
Treatment Options for Urinary Tract Infection (UTI)
The treatment for a Urinary Tract Infection (UTI) primarily involves antibiotics, but the specific type, dosage, and duration depend on the severity of the infection, the type of bacteria identified, and individual patient factors. It’s crucial to complete the full course of antibiotics, even if symptoms improve, to ensure the infection is fully eradicated and to prevent recurrence or antibiotic resistance.
Antibiotics: The Primary Treatment
Your doctor will prescribe antibiotics based on the urine culture results. Common antibiotics used for UTIs include:
- Trimethoprim/sulfamethoxazole (Bactrim, Septra): A common first-line treatment.
- Fosfomycin (Monurol): Often given as a single dose for uncomplicated UTIs.
- Nitrofurantoin (Macrodantin, Macrobid): Another common choice for lower UTIs.
- Cephalexin (Keflex): A broader-spectrum antibiotic.
- Ceftriaxone (Rocephin): May be used for more severe or complicated UTIs, sometimes intravenously.
- Fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin): Generally reserved for more severe UTIs or when other antibiotics are ineffective, due to concerns about side effects.
The duration of treatment can range from a single dose for uncomplicated UTIs to 7-14 days or longer for more severe or complicated infections, such as kidney infections. For mild, uncomplicated UTIs, symptoms often improve within a few days of starting treatment. However, it’s essential to finish the entire prescription to prevent recurrence.
Pain Relief and Symptom Management
While antibiotics work to clear the infection, you might still experience discomfort. Your doctor may also recommend:
- Pain Relievers: Over-the-counter pain relievers such as ibuprofen (Advil, Motrin IB) or acetaminophen (Tylenol) can help manage pain and fever.
- Urinary Pain Relievers: Phenazopyridine (Pyridium) can help numb the lining of the urinary tract, providing relief from burning and urgency. This medication can turn urine orange or red.
For more details on treatments, the CDC provides guidelines on antibiotic use for UTIs.
Treatment for Recurrent UTIs
For individuals experiencing recurrent UTIs (typically three or more in a year), your doctor might suggest a different approach:
- Low-Dose Antibiotics: A low dose of antibiotics taken daily for six months or longer.
- Postcoital Dosing: Taking a single dose of antibiotic after sexual intercourse.
- Vaginal Estrogen Therapy: For postmenopausal women, vaginal estrogen cream can help restore the normal vaginal flora.
- Self-Treatment: In some cases, your doctor might provide a prescription for antibiotics to start at home as soon as symptoms appear.
When to Seek Emergency Care
If you develop symptoms of a kidney infection (high fever, severe back pain, nausea, vomiting) or if your UTI symptoms worsen despite treatment, seek immediate medical attention. These could indicate a spreading infection that requires urgent intervention.
Always consult with a healthcare professional for diagnosis and treatment of a Urinary Tract Infection (UTI). Self-treating can lead to complications and delay proper care.
Preventing Urinary Tract Infection (UTI): Proactive Strategies
While not all UTIs can be prevented, especially in individuals with specific risk factors, many simple yet effective strategies can significantly reduce your chances of developing a Urinary Tract Infection (UTI). These strategies focus on maintaining good hygiene, promoting healthy urinary habits, and supporting overall urinary tract health.
Lifestyle and Hygiene Practices
- Drink Plenty of Fluids: Staying well-hydrated, particularly with water, helps dilute urine and ensures more frequent urination, which flushes bacteria out of the urinary tract before they can cause an infection. Aim for at least 8-10 glasses of water daily.
- Wipe from Front to Back: This is crucial for women. Wiping from front to back after urinating and bowel movements prevents bacteria from the anal region from spreading to the urethra and vagina.
- Urinate After Intercourse: Urinating shortly after sexual activity helps flush out any bacteria that may have entered the urethra during sex.
- Avoid Irritating Feminine Products: Steer clear of douches, deodorant sprays, scented powders, and other feminine products that can irritate the urethra and alter the natural balance of vaginal bacteria.
- Choose Appropriate Underwear: Wear cotton underwear and loose-fitting clothing. Cotton allows for better airflow, keeping the area dry and preventing bacterial growth, unlike synthetic fabrics that trap moisture.
- Change Pads/Tampons Frequently: During menstruation, change sanitary products regularly to prevent bacterial overgrowth.
- Shower Instead of Bathe: While not a strict rule, some experts suggest showering rather than taking baths, as sitting in bathwater can potentially expose the urethra to bacteria.
Dietary and Supplement Considerations
- Cranberry Products: While research on cranberry’s effectiveness is mixed, some studies suggest that compounds in cranberries (proanthocyanidins) may prevent bacteria from adhering to the urinary tract walls. Cranberry juice (unsweetened) or supplements might be helpful for some individuals, though they are not a substitute for medical treatment once an infection has occurred.
- Probiotics: Some evidence suggests that probiotics, particularly those containing Lactobacillus strains, may help maintain a healthy balance of bacteria in the vagina and urinary tract, potentially reducing UTI risk.
Managing Specific Risk Factors
- Manage Diabetes: If you have diabetes, maintaining good blood sugar control is essential, as high blood sugar can increase UTI risk.
- Address Bladder Issues: For individuals with urinary incontinence or other bladder issues, work with your doctor to manage these conditions effectively.
- Postmenopausal Women: Discuss vaginal estrogen therapy with your doctor, as it can help prevent recurrent UTIs by restoring vaginal flora.
By adopting these preventive measures, you can significantly reduce your risk of developing a Urinary Tract Infection (UTI) and maintain better urinary health. For further guidance on prevention, the WebMD guide to understanding UTIs offers valuable insights.
Complications of Untreated Urinary Tract Infection (UTI)
While most uncomplicated Urinary Tract Infections (UTIs) are easily treatable with antibiotics, neglecting symptoms or failing to complete a full course of medication can lead to serious and potentially life-threatening complications. Understanding these risks underscores the importance of prompt diagnosis and adherence to treatment plans.
Potential Complications
- Recurrent Infections: One of the most common complications is the development of recurrent UTIs. In some cases, the initial infection isn’t fully cleared, or underlying risk factors persist, leading to repeated episodes. This can be frustrating and significantly impact quality of life.
- Kidney Damage (Chronic Pyelonephritis): If a bladder infection spreads to the kidneys (pyelonephritis) and is left untreated or inadequately treated, it can cause permanent kidney damage. Chronic kidney infections can lead to scarring, impaired kidney function, and in severe cases, kidney failure.
- Sepsis: This is a life-threatening complication where the infection spreads from the urinary tract into the bloodstream, triggering a severe inflammatory response throughout the body. Sepsis can lead to organ damage, septic shock, and death if not treated urgently. Symptoms include high fever, chills, rapid heartbeat, rapid breathing, and confusion.
- Premature Birth and Low Birth Weight (in pregnant women): UTIs during pregnancy pose significant risks to both the mother and the fetus. Untreated UTIs can lead to kidney infections, which are associated with an increased risk of premature labor and delivery, as well as low birth weight in infants.
- Urethral Narrowing (Stricture) in Men: While less common, recurrent or severe urethritis (inflammation of the urethra) in men can sometimes lead to urethral strictures, making urination difficult.
It’s important to take any suspected Urinary Tract Infection (UTI) seriously and seek medical advice. Even if symptoms seem to resolve on their own, the bacteria might still be present, leading to a more severe infection later. Never underestimate the potential for a seemingly minor infection to escalate into a major health crisis. For more on potential complications, the NHS provides information on UTI complications.
Urinary Tract Infection (UTI) in Specific Populations
While UTIs are common, their presentation, diagnosis, and management can differ significantly across various demographic groups. Understanding these nuances is crucial for tailored and effective care.
Women
Women are disproportionately affected by UTIs, with about 50-60% experiencing at least one in their lifetime. This is primarily due to their shorter urethra and its proximity to the anus. Factors like sexual activity, certain types of birth control (diaphragms, spermicides), and menopause (due to decreased estrogen) significantly increase risk. Recurrent UTIs are also more common in women, often necessitating long-term preventive strategies or specialized evaluation.
Men
UTIs are less common in men, especially younger men, but their occurrence often signals an underlying issue. In older men, an enlarged prostate (benign prostatic hyperplasia, BPH) is a frequent cause, as it can obstruct urine flow and prevent complete bladder emptying. Other causes in men include kidney stones, urinary tract abnormalities, or catheter use. When a man gets a UTI, it’s often considered a complicated UTI and warrants a thorough investigation to identify and address the root cause.
Children
UTIs in children can be challenging to diagnose because symptoms may be non-specific, such as fever, irritability, poor feeding, vomiting, or unexplained wetting accidents. Prompt diagnosis and treatment are vital in children, as untreated UTIs can lead to kidney scarring and long-term kidney problems. Imaging studies (like ultrasound) are often recommended after a child’s first UTI to check for any anatomical abnormalities in the urinary tract that might predispose them to infections.
Elderly Individuals
Older adults are more susceptible to UTIs due to a variety of factors, including weakened immune systems, decreased bladder emptying efficiency, incontinence, catheter use, and conditions like diabetes or prostate enlargement in men. Atypical symptoms are common in the elderly; they may not report classic burning or frequency but instead experience confusion, delirium, falls, or general weakness. This can make diagnosis difficult, leading to delayed treatment and increased risk of severe complications like sepsis.
Pregnant Women
Pregnant women are at an increased risk of UTIs due to hormonal changes and the pressure of the growing uterus on the bladder, which can hinder complete bladder emptying. Asymptomatic bacteriuria (bacteria in the urine without symptoms) is also common during pregnancy and, if left untreated, can progress to kidney infections, premature labor, and low birth weight. Therefore, pregnant women are typically screened for UTIs early in pregnancy, and any infection is treated promptly with antibiotics safe for pregnancy.
Tailoring diagnostic approaches and treatment plans to these specific populations ensures better outcomes and reduces the risk of complications from a Urinary Tract Infection (UTI).
Debunking Common Myths About Urinary Tract Infection (UTI)
Misinformation about Urinary Tract Infections (UTIs) is widespread, often leading to delayed treatment, inappropriate self-care, or unnecessary anxiety. Let’s clarify some common misconceptions surrounding UTIs.
Myth 1: UTIs are only caused by poor hygiene.
Fact: While poor hygiene can contribute to UTIs by facilitating bacterial transfer, it’s far from the only cause. Anatomical factors, sexual activity, genetics, hormonal changes (like menopause), diabetes, and certain medical conditions or procedures are significant risk factors. Even individuals with excellent hygiene can get a Urinary Tract Infection (UTI).
Myth 2: Cranberry juice always cures a UTI.
Fact: Cranberry products may help prevent UTIs in some individuals by inhibiting bacteria from adhering to the bladder wall, but they are generally not effective as a treatment once an infection has taken hold. If you suspect a UTI, you need to see a doctor for diagnosis and antibiotic treatment. Relying solely on cranberry juice can delay proper medical care and lead to complications.
Myth 3: Only women get UTIs.
Fact: While UTIs are significantly more common in women, men, children, and even infants can get them. In men, UTIs are less common but often indicate an underlying issue, such as an enlarged prostate or kidney stones, requiring thorough investigation. Similarly, UTIs in children warrant careful evaluation.
Myth 4: A UTI is a sexually transmitted infection (STI).
Fact: A Urinary Tract Infection (UTI) is an infection of the urinary system, most commonly caused by bacteria from the gut (like E. coli). While sexual activity can sometimes introduce bacteria into the urethra and increase the risk of a UTI, a UTI itself is not an STI. STIs are infections passed from person to person through sexual contact and affect the reproductive organs or other areas. It is possible to have both an STI and a UTI simultaneously, as their symptoms can sometimes overlap.
Myth 5: You can always tell if you have a UTI.
Fact: While many UTIs present with classic symptoms like burning during urination and frequent urges, some can be asymptomatic (especially common in pregnant women and elderly individuals). In older adults, UTIs might manifest as confusion, agitation, or falls without any urinary symptoms. This is why regular screening is important for certain at-risk groups.
Myth 6: UTIs are not serious.
Fact: While uncomplicated UTIs are easily treated, untreated or severe UTIs can lead to serious complications, including kidney infections (pyelonephritis), permanent kidney damage, and even sepsis, a life-threatening bloodstream infection. It’s crucial to seek medical attention for suspected UTIs.
Understanding these facts can empower individuals to make informed decisions about their health and seek appropriate care for a Urinary Tract Infection (UTI) when needed.
Managing Recurrent Urinary Tract Infections (UTIs)
Recurrent UTIs, defined as two or more UTIs within six months or three or more within a year, can be a frustrating and debilitating issue for many individuals, particularly women. Managing these persistent infections often requires a multi-faceted approach beyond standard antibiotic treatment. The goal is to identify underlying causes, prevent future episodes, and improve quality of life.
Identifying Underlying Causes
For recurrent UTIs, your healthcare provider will likely conduct a more thorough investigation to rule out contributing factors:
- Detailed Medical History: Reviewing lifestyle, sexual habits, contraception, and past medical conditions.
- Urine Culture and Sensitivity: Essential to identify specific bacteria and their antibiotic resistance patterns.
- Imaging Studies: Ultrasound, CT scan, or MRI may be used to check for structural abnormalities, kidney stones, or other blockages in the urinary tract.
- Cystoscopy: A procedure to visualize the bladder and urethra directly, looking for abnormalities like strictures, polyps, or inflammation.
- Post-Void Residual (PVR) Measurement: To check if the bladder is emptying completely after urination.
Preventive Strategies for Recurrent UTIs
Once underlying causes are addressed, various preventive strategies can be employed:
- Prophylactic Antibiotics: This is a common approach. It involves taking low-dose antibiotics daily for several months, or a single dose after sexual intercourse (postcoital prophylaxis), or self-starting a short course of antibiotics at the first sign of symptoms.
- Non-Antibiotic Strategies:
- D-Mannose: A type of sugar that can prevent E. coli from adhering to urinary tract walls.
- Cranberry Products: As mentioned, may reduce bacterial adhesion.
- Probiotics: Specifically Lactobacillus strains, to restore healthy vaginal flora.
- Vaginal Estrogen: For postmenopausal women, topical estrogen can restore vaginal pH and flora, making the urinary tract less susceptible to infection.
- Increased Fluid Intake: Continues to be a cornerstone of prevention.
- Good Hygiene Practices: Reinforcing front-to-back wiping, urinating after sex.
- Immunotherapy (Vaccines): In some regions, a bacterial lysate vaccine (e.g., Uro-Vaxom) is available and may be considered for patients with recurrent UTIs to boost the immune response.
- Surgical Correction: If a structural abnormality is identified (e.g., vesicoureteral reflux, urinary tract obstruction), surgical intervention might be necessary to correct the problem and reduce UTI recurrence.
Working closely with a healthcare provider, often a urologist or gynecologist, is essential to develop a personalized management plan for recurrent Urinary Tract Infection (UTI). This collaborative approach ensures that all potential contributing factors are considered and the most effective preventive measures are implemented to break the cycle of repeated infections.
The Role of Diet and Hydration in Urinary Tract Health
Beyond medical treatments, daily habits, particularly related to diet and hydration, play a significant role in maintaining overall urinary tract health and can be crucial in both preventing and managing Urinary Tract Infection (UTI). What you consume directly impacts the composition of your urine and the environment within your urinary system.
Hydration: Your First Line of Defense
Adequate fluid intake is arguably the single most important dietary factor for urinary tract health. Water is your best friend:
- Flushing Bacteria: Drinking plenty of water helps to dilute your urine and increases the frequency of urination. This mechanical flushing action helps to remove bacteria from the urinary tract before they have a chance to multiply and cause an infection.
- Diluting Irritants: Diluted urine is also less irritating to the bladder lining, which can be beneficial during an active infection or for sensitive bladders.
- Preventing Stone Formation: Good hydration also helps prevent the formation of kidney stones, which can sometimes block urine flow and increase UTI risk.
Aim for clear or very pale yellow urine as an indicator of adequate hydration. While other fluids like herbal teas and clear broths contribute, water should be your primary choice.
Dietary Considerations
Certain foods and drinks can either support or hinder urinary tract health:
- Foods to Emphasize:
- High-Fiber Foods: Whole grains, fruits, and vegetables can help prevent constipation, which can sometimes put pressure on the bladder and impede complete emptying, potentially contributing to UTIs.
- Probiotic-Rich Foods: Yogurt, kefir, and fermented foods containing beneficial bacteria can support a healthy microbiome, particularly in the gut and vagina, which can indirectly protect against UTIs.
- Antioxidant-Rich Foods: Berries (including cranberries), leafy greens, and other fruits and vegetables provide antioxidants that support overall immune health.
- Foods/Drinks to Limit or Avoid (especially during a UTI):
- Caffeine: Found in coffee, tea, and some sodas, caffeine is a diuretic and a bladder irritant. It can worsen urgency, frequency, and discomfort during a UTI.
- Alcohol: Also a diuretic and irritant, alcohol can dehydrate you and exacerbate UTI symptoms.
- Sugary Drinks: High sugar intake can potentially feed bacteria and contribute to an unhealthy microbial balance.
- Spicy Foods: Can irritate the bladder lining in some individuals.
- Acidic Foods/Drinks: Citrus fruits and juices (other than possibly cranberry), tomatoes, and vinegar can sometimes irritate a sensitive bladder.
It’s important to note that individual sensitivities vary. Pay attention to how your body reacts to different foods and adjust your diet accordingly. While diet and hydration are excellent supportive measures, they are not a substitute for medical treatment when a Urinary Tract Infection (UTI) is present.
The Link Between Sexual Health and Urinary Tract Infection (UTI)
Sexual activity is a significant risk factor for Urinary Tract Infection (UTI), particularly in women. Understanding this connection is essential for both prevention and managing recurrent infections. It’s not about avoiding sex, but rather adopting practices that minimize bacterial transfer and support urinary tract health.
How Sexual Activity Increases UTI Risk
- Bacterial Introduction: During sexual intercourse, bacteria from the vaginal or anal area can be massaged into the urethra. The shorter female urethra makes this transfer particularly easy.
- Friction: Friction during sex can push bacteria further up the urethra towards the bladder.
- Spermicides and Diaphragms: Certain birth control methods, such as diaphragms and spermicides, can alter the natural bacterial balance in the vagina, making it easier for UTI-causing bacteria to thrive and ascend the urinary tract.
Preventive Measures Related to Sexual Activity
Adopting these habits can significantly reduce the risk of post-coital UTIs:
- Urinate Before and Immediately After Sex: Urinating before sex can help empty the bladder, and urinating immediately after sex helps flush out any bacteria that may have entered the urethra during intercourse. This is one of the most effective preventive measures.
- Stay Hydrated: Drinking water before and after sex can help ensure a good urine flow to aid in flushing bacteria.
- Proper Hygiene: Washing the genital area before and after sex can help reduce the bacterial load, though excessive washing or harsh soaps should be avoided as they can cause irritation.
- Reconsider Contraception: If you experience recurrent UTIs and use diaphragms or spermicides, discuss alternative birth control methods with your doctor.
- Lubrication: Adequate lubrication during sex can reduce friction and potential irritation to the urethra.
- Communicate with Partner: Ensuring good hygiene for both partners can also contribute to reducing bacterial transfer.
It’s important to reiterate that while there’s a clear link between sexual activity and UTIs, a Urinary Tract Infection (UTI) is not an STI. However, some STI symptoms can mimic UTI symptoms, so if you’re unsure or have new partners, it’s always wise to consult a healthcare provider for accurate diagnosis and testing.
When to See a Doctor for a Urinary Tract Infection (UTI)
Knowing when to seek medical attention for a suspected Urinary Tract Infection (UTI) is crucial for preventing complications and ensuring effective treatment. While some mild symptoms might tempt you to wait, prompt diagnosis and intervention are always recommended.
Immediate Medical Attention is Recommended If:
- You Experience UTI Symptoms: Any new onset of burning during urination, frequent urination, urgency, pelvic pain, or cloudy/bloody urine warrants a doctor’s visit. Self-diagnosis and self-treatment can be dangerous.
- Symptoms Worsen or Don’t Improve: If your symptoms don’t start to improve within a day or two of starting antibiotics, or if they get worse, contact your doctor.
- Symptoms of a Kidney Infection Develop: This is an emergency. Seek immediate medical care if you have:
- High fever (101°F or higher)
- Chills and shaking
- Nausea and vomiting
- Severe back or flank pain (pain in your side, just below your ribs)
- You Are Pregnant: UTIs during pregnancy can lead to serious complications for both mother and baby. Always get tested and treated promptly.
- You Have Diabetes or a Weakened Immune System: These conditions increase the risk of complicated UTIs and severe outcomes.
- You Are a Man or a Child: UTIs in men and children are less common and often indicate an underlying issue that needs investigation.
- You Experience Recurrent UTIs: If you have frequent UTIs, your doctor can help identify underlying causes and develop a long-term prevention strategy.
- You Have Blood in Your Urine: While sometimes a UTI symptom, blood in the urine can also indicate other serious conditions, so it warrants medical evaluation.
Never ignore symptoms of a Urinary Tract Infection (UTI). Early intervention is key to a swift recovery and preventing more severe health problems. A healthcare professional can accurately diagnose the infection, identify the responsible bacteria, and prescribe the most effective treatment, ensuring you get back to feeling well as quickly and safely as possible.
Comparing Different Approaches to UTI Management
Managing a Urinary Tract Infection (UTI) involves various strategies, from immediate medical intervention to long-term preventive measures. Understanding the differences between these approaches can help individuals make informed decisions in consultation with their healthcare providers.
Acute Treatment vs. Prevention
Acute Treatment: This focuses on eliminating an active infection. It almost always involves antibiotics, prescribed based on the type of bacteria and its susceptibility. The goal is rapid symptom relief and preventing the infection from spreading to the kidneys or bloodstream. It’s a reactive approach to an existing problem.
Prevention: This involves proactive strategies to reduce the likelihood of developing a UTI in the first place, or preventing recurrent UTIs. This includes lifestyle changes (hydration, hygiene), dietary adjustments, and sometimes low-dose antibiotics or non-antibiotic supplements. Prevention is a long-term strategy aimed at maintaining urinary tract health.
Conventional vs. Complementary Approaches
Conventional Medicine: The cornerstone of UTI treatment is antibiotics, which are highly effective at killing the bacteria causing the infection. Diagnosis relies on laboratory tests like urinalysis and urine culture. This approach is evidence-based and critical for serious infections.
Complementary Approaches: These include natural remedies, herbal supplements (like cranberry or D-Mannose), and probiotics. While some show promise in preventing UTIs or supporting urinary health, they are generally not recommended as standalone treatments for an active infection. They can be beneficial as adjuncts to conventional treatment or as part of a preventive regimen, but always discuss them with your doctor to ensure safety and efficacy, especially to avoid interactions with prescribed medications.
Short-Term vs. Long-Term Management
Short-Term Management: For an uncomplicated, first-time UTI, a short course of antibiotics (3-7 days) is typically sufficient. Symptomatic relief with pain relievers is also part of short-term management.
Long-Term Management: For recurrent UTIs, a more extensive long-term strategy is required. This might involve extended low-dose antibiotics, vaginal estrogen therapy for postmenopausal women, consistent use of D-Mannose or probiotics, or addressing underlying anatomical issues. The goal is to break the cycle of recurrence and improve sustained urinary health.
The table below summarizes key aspects of UTI management:
| Aspect | Acute Treatment (Active UTI) | Preventive Measures (Reducing Risk) | Recurrent UTI Management |
|---|---|---|---|
| Primary Goal | Eradicate existing infection, relieve symptoms | Avoid new infections | Break cycle of infections, improve quality of life |
| Main Intervention | Prescription Antibiotics | Hydration, Hygiene, Lifestyle changes | Long-term low-dose antibiotics, D-Mannose, Probiotics, Vaginal Estrogen, Surgical correction |
| Key Diagnostic Tests | Urinalysis, Urine Culture | Identification of risk factors (e.g., sexual habits, medical conditions) | Detailed work-up: Imaging, Cystoscopy, PVR, specialized cultures |
| Speed of Relief | Typically within 24-48 hours | Gradual, long-term benefit | Variable, depending on strategy and individual |
| Risk if Untreated | Kidney infection, Sepsis, Chronic damage | Increased likelihood of developing a UTI | Persistent discomfort, potential kidney damage, antibiotic resistance |
| Role of Doctor | Essential for diagnosis and prescription | Guidance on best practices, screening | Crucial for comprehensive evaluation and personalized plan |
It is important to remember that all approaches should be discussed with a healthcare professional to ensure they are appropriate for your specific situation and health needs. A holistic approach, integrating medical treatment with lifestyle modifications, often yields the best outcomes for a Urinary Tract Infection (UTI).
Frequently Asked Questions (FAQs) about Urinary Tract Infection (UTI)
Can UTIs go away on their own without antibiotics?
While very mild UTIs might occasionally resolve on their own, especially in individuals with strong immune systems and excellent hydration, it’s generally not recommended to wait. Most UTIs require antibiotics to effectively clear the bacterial infection. Delaying treatment can lead to the infection spreading to the kidneys, causing more severe complications like pyelonephritis or even sepsis. Always consult a doctor if you suspect a UTI.
Is a UTI contagious?
No, a Urinary Tract Infection (UTI) is not considered contagious in the way a cold or flu is. It’s an internal infection caused by bacteria, usually from your own gut, entering your urinary tract. You cannot catch a UTI from another person through casual contact or sharing toilets. While sexual activity can sometimes introduce bacteria into the urethra and increase the risk of a UTI, the infection itself is not passed sexually from one person to another.
Can stress cause a UTI?
Stress itself does not directly cause a UTI. However, chronic stress can weaken the immune system, making your body less effective at fighting off infections, including bacterial invasions in the urinary tract. Stress can also lead to changes in habits, such as poor hydration or infrequent urination, which can indirectly increase UTI risk. So, while not a direct cause, stress can be a contributing factor.
What’s the difference between a UTI and a yeast infection?
Both UTIs and yeast infections affect the genital area and can cause discomfort, but they are distinct conditions. A Urinary Tract Infection (UTI) is a bacterial infection of the urinary system (bladder, urethra, kidneys), causing symptoms like burning during urination, frequent urges, and pelvic pain. A yeast infection (candidiasis) is a fungal infection, typically of the vagina, caused by an overgrowth of Candida yeast. Symptoms include intense itching, irritation, thick white discharge, and sometimes burning, but usually not specifically during urination unless the vulva is irritated. They require different treatments.
Can men get UTIs?
Yes, men can absolutely get UTIs, although they are much less common than in women. When a man gets a UTI, especially a younger man, it often indicates an underlying issue in the urinary tract, such as an enlarged prostate, kidney stones, or structural abnormalities. Therefore, a UTI in a man usually warrants a more thorough investigation by a healthcare provider to identify and address the root cause.
How long does it take for antibiotics to work for a UTI?
Most people start to feel significant relief from UTI symptoms within 24 to 48 hours of starting antibiotics. However, it is crucial to complete the entire course of antibiotics as prescribed by your doctor, even if your symptoms disappear. Stopping early can lead to the infection recurring, becoming more difficult to treat, or contributing to antibiotic resistance.
Can certain foods or drinks make a UTI worse?
Yes, certain foods and drinks can irritate the bladder and potentially worsen UTI symptoms, especially during an active infection. Common culprits include caffeine (coffee, tea, soda), alcohol, highly acidic foods (citrus fruits, tomatoes), and spicy foods. While not directly causing the infection, avoiding these can help reduce discomfort. Staying well-hydrated with water is generally recommended.
Conclusion: Prioritizing Your Urinary Health
Understanding and proactively managing Urinary Tract Infection (UTI) is paramount for maintaining overall health and well-being. From recognizing the subtle cues of an early infection to implementing robust preventive strategies, being informed empowers you to take control. Remember that while common, UTIs are not to be taken lightly; prompt medical attention for symptoms and adherence to treatment plans are crucial to prevent serious complications like kidney damage or sepsis. By prioritizing hydration, practicing good hygiene, addressing risk factors, and consulting healthcare professionals for recurrent issues, you can significantly reduce your vulnerability to this often-distressing condition. Stay vigilant, stay informed, and commit to safeguarding your urinary health for a more comfortable and healthier life. If you suspect a UTI, don’t hesitate to consult your doctor for proper diagnosis and treatment.







