Depression is a formidable adversary, affecting millions worldwide and casting a long shadow over daily life. While conventional treatments like medication and psychotherapy offer relief for many, a significant portion of individuals still struggle to find lasting solutions. This often leads to a search for innovative, non-invasive approaches that address the root causes of mood dysregulation. Enter neurofeedback – a cutting-edge brain training technique that is gaining significant traction as a powerful tool in the fight against depression.

Imagine being able to gently guide your brain to healthier, more balanced patterns, reducing the grip of sadness, anhedonia, and low energy. That’s the promise of neurofeedback for depression. This comprehensive guide will explore the science behind this fascinating therapy, delve into its benefits, walk you through the treatment process, and help you understand if it might be the missing piece in your journey towards mental wellness. We’ll uncover how EEG biofeedback for depression works, examine its effectiveness, and provide you with the information you need to make informed decisions about this innovative approach to mood regulation.
Understanding Depression: More Than Just a Feeling
Depression is far more complex than simply feeling sad. It’s a serious mood disorder characterized by persistent feelings of sadness, loss of interest or pleasure, changes in appetite or sleep, fatigue, difficulty concentrating, feelings of worthlessness or guilt, and sometimes thoughts of self-harm. These symptoms can significantly impair daily functioning, affecting relationships, work, and overall quality of life.
While life events, genetics, and psychological factors play a role, modern neuroscience increasingly points to biological underpinnings, particularly in the brain. Research suggests that depression is associated with imbalances in neurotransmitters (like serotonin, dopamine, and norepinephrine) and dysregulation in specific brain circuits responsible for mood, emotion regulation, and cognitive function. Crucially, patterns of brainwave activity, measured by an electroencephalogram (EEG), often show distinct deviations in individuals experiencing depression. These abnormal brainwave patterns can contribute to symptoms such as rumination, difficulty with emotional processing, and impaired executive function, highlighting why brainwave training depression can be so impactful.
What is Neurofeedback? The Basics of Brainwave Training
Neurofeedback, also known as EEG biofeedback, is a non-invasive form of brain training that helps individuals learn to self-regulate their brainwave activity. Think of it as a workout for your brain, where you learn to optimize its performance. The core principle is operant conditioning: your brain learns to produce more desirable brainwave patterns and reduce undesirable ones through real-time feedback.
During a typical neurofeedback session, sensors are placed on your scalp to measure your brain’s electrical activity (brainwaves). This activity is then displayed on a computer screen in real-time. As your brain produces the desired brainwave patterns, you receive positive feedback – perhaps a video game character moves, a movie plays smoothly, or a sound tone is emitted. Conversely, if your brain produces undesirable patterns, the feedback stops or changes, signaling to your brain to adjust. Over time, with consistent practice, your brain learns to maintain these healthier patterns independently, leading to lasting changes in mood, focus, and overall well-being. This process is fundamental to understanding how neurofeedback works for depression.

How Neurofeedback Specifically Targets Depression
The beauty of neurofeedback lies in its ability to directly address the brainwave dysregulation often associated with depression. Research has identified several common brainwave patterns linked to depressive symptoms:
- Excessive Alpha Waves in the Frontal Lobe: Often associated with reduced cognitive flexibility, difficulty initiating tasks, and a sense of being “stuck.”
- Asymmetry in Alpha Waves: Specifically, higher alpha activity in the right frontal lobe compared to the left, which is linked to negative emotional states, withdrawal, and decreased positive affect.
- Excessive Theta Waves: Can be associated with brain fog, difficulty concentrating, and a dreamy or spaced-out feeling.
- Low Beta Waves: Sometimes linked to fatigue, lack of motivation, and difficulty with mental processing.
Neurofeedback protocols for depression are tailored to correct these specific imbalances. For example, a common protocol aims to increase alpha waves in the left frontal lobe while decreasing them in the right, or to reduce excessive theta activity. By training the brain to produce more optimal brainwave patterns, neurofeedback helps to:
- Improve mood regulation and emotional resilience.
- Increase focus, concentration, and cognitive clarity.
- Reduce rumination and negative thought patterns.
- Enhance sleep quality and energy levels.
- Alleviate symptoms of anxiety often co-occurring with depression.
This targeted approach leverages the brain’s natural neuroplasticity – its ability to reorganize itself by forming new neural connections throughout life. Through repeated neurofeedback sessions, the brain learns and strengthens these healthier pathways, leading to more stable and positive emotional states. It’s a fundamental shift in how the brain operates, offering sustainable relief from the persistent symptoms of depression.
The Neurofeedback Process: What to Expect
Embarking on neurofeedback therapy for depression typically involves a structured process designed to personalize the treatment to your unique brain and symptoms.
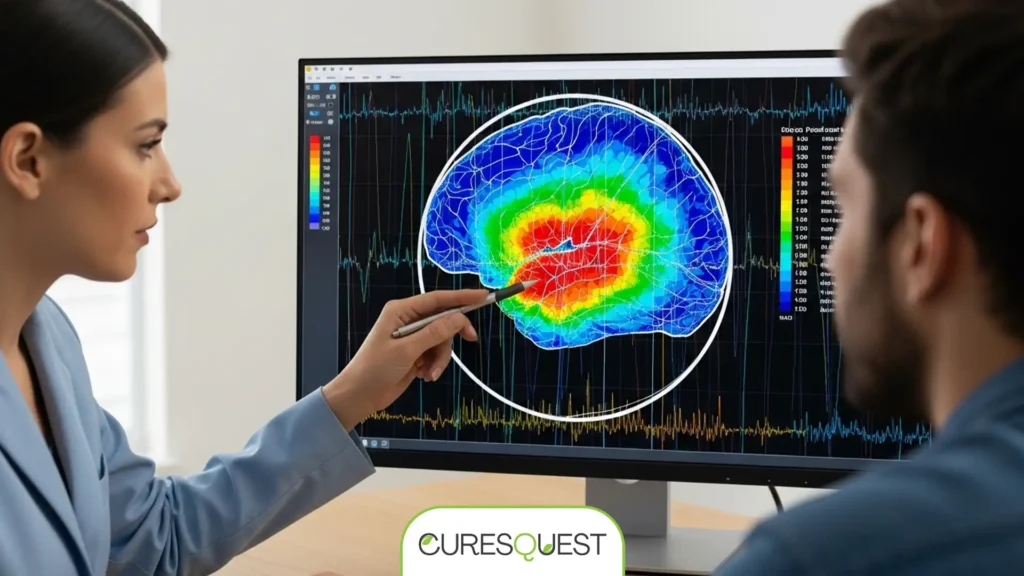
Initial Assessment: QEEG Brain Mapping
The journey usually begins with a quantitative electroencephalogram (QEEG), often referred to as “brain mapping.” During this non-invasive procedure, a cap fitted with electrodes is placed on your head to record your brain’s electrical activity. This raw EEG data is then processed by specialized software, comparing your unique brainwave patterns to a normative database of healthy brains. The QEEG identifies specific areas of dysregulation – where your brain is over- or under-performing – that are contributing to your depressive symptoms. This detailed map is crucial for designing a highly individualized neurofeedback protocol, ensuring the training is precisely targeted to your needs.
Neurofeedback Sessions
Once your QEEG assessment is complete, your practitioner will develop a personalized training plan. A typical neurofeedback session lasts between 30 to 60 minutes. You’ll sit comfortably in a chair, and sensors will be placed on your scalp, usually connected to an amplifier and a computer. These sensors simply read your brainwaves; they do not send any electrical current into your brain.
You’ll then engage with a computer screen, watching a movie, playing a simple video game, or listening to sounds. The software detects when your brain produces the desired brainwave patterns (e.g., increasing alpha in the left frontal lobe) and provides immediate positive feedback – the movie plays, the game moves forward, or the sound becomes clearer. When your brain drifts into undesirable patterns, the feedback stops or changes, prompting your brain to adjust. This real-time, continuous feedback allows your brain to learn and self-correct, gradually shifting towards healthier, more balanced activity.
Duration and Frequency
The number of sessions required varies depending on the individual, the severity of depression, and how quickly your brain responds to training. Most treatment plans involve 20 to 40 sessions, typically scheduled 2-3 times per week initially. Consistency is key to achieving lasting results, as the brain needs repeated exposure to learn and solidify new patterns. Your progress will be regularly monitored, often with follow-up QEEGs, to ensure the protocols remain effective and to make any necessary adjustments.
Benefits of Neurofeedback for Depression
The growing interest in neurofeedback for depression stems from its unique advantages, offering hope to those who haven’t found sufficient relief through conventional methods. Here are some key benefits:
- Non-Invasive and Drug-Free: Neurofeedback does not involve medication, electrical currents, or any invasive procedures, making it a safe option for many, including those sensitive to pharmaceutical side effects or seeking alternative depression therapies.
- Sustainable, Long-Term Results: Unlike medications that manage symptoms, neurofeedback trains the brain to self-regulate. This learning process leads to neuroplastic changes, meaning the brain actually reorganizes itself. Once these healthier patterns are established, the benefits are often sustained long after treatment ends.
- Improved Mood and Emotional Regulation: By targeting specific brainwave imbalances, neurofeedback can significantly reduce feelings of sadness, hopelessness, and irritability, fostering a more positive and stable emotional state.
- Enhanced Cognitive Function: Many individuals with depression experience “brain fog,” difficulty concentrating, and memory issues. Neurofeedback can improve focus, attention, and overall cognitive clarity.
- Better Sleep Quality: Sleep disturbances are common with depression. By normalizing brainwave patterns, neurofeedback often leads to improved sleep onset, duration, and quality.
- Reduced Anxiety and Stress: Depression frequently co-occurs with anxiety. Neurofeedback protocols can simultaneously address anxiety symptoms, leading to a calmer and more resilient nervous system.
- Complementary to Other Treatments: Neurofeedback can be effectively integrated with psychotherapy (like CBT or DBT) and even medication, potentially enhancing the efficacy of other interventions and sometimes allowing for reduced medication dosages under medical supervision.
- Addresses Root Causes: Rather than just masking symptoms, neurofeedback works to correct underlying brain dysregulation, offering a more fundamental approach to mental wellness.
Is Neurofeedback Effective for Depression? Research and Evidence
The scientific community has been increasingly focused on understanding the efficacy of neurofeedback for depression. While more large-scale, randomized controlled trials are always beneficial, existing research, including numerous clinical studies and meta-analyses, provides compelling evidence for its effectiveness.
Studies often highlight significant reductions in depressive symptoms, sometimes comparable to or even exceeding those seen with medication or psychotherapy alone. For instance, research published in journals like Clinical EEG and Neuroscience and Applied Psychophysiology and Biofeedback has demonstrated that specific neurofeedback protocols, particularly those targeting frontal alpha asymmetry or theta/beta ratios, can lead to clinically meaningful improvements in mood, sleep, and overall functioning for individuals with major depressive disorder. Meta-analyses pooling data from multiple studies generally conclude that neurofeedback is a promising and effective non-pharmacological depression treatment.
The success rates for neurofeedback for depression vary, but many clinics report that 70-80% of clients experience significant improvement in their symptoms. This is often attributed to the personalized nature of QEEG-guided neurofeedback, which allows for precise targeting of individual brain dysregulations. Patients often report not just a reduction in symptoms but also a greater sense of well-being, increased resilience, and an improved ability to cope with stress.
However, it’s important to acknowledge that neurofeedback is not a guaranteed cure for everyone, and individual responses can vary. Factors such as the severity and chronicity of depression, co-occurring conditions, the skill of the practitioner, and patient commitment all play a role in outcomes. Nevertheless, the consistent positive findings in research and clinical practice position neurofeedback as a valuable and evidence-based option for those seeking effective depression treatment.
Comparing Treatment Approaches for Depression
To provide a clearer perspective, here’s a comparative overview of neurofeedback alongside other common depression treatments:
| Treatment Method | Mechanism of Action | Typical Efficacy (General) | Potential Side Effects | Duration/Commitment | Long-Term Sustainability |
|---|---|---|---|---|---|
| Neurofeedback | Trains brain to self-regulate brainwave patterns, enhancing neuroplasticity. | Good to Excellent (70-80% symptom reduction reported clinically). | Mild (fatigue, agitation, headache initially), generally well-tolerated. | 20-40 sessions, 2-3 times/week. | High (brain learns new patterns). |
| Antidepressant Medication | Alters neurotransmitter levels in the brain. | Moderate to Good (40-60% achieve remission). | Nausea, weight gain, sexual dysfunction, insomnia, emotional blunting. | Daily, ongoing. | Dependent on continuous use. |
| Psychotherapy (CBT/DBT) | Teaches coping skills, challenges negative thought patterns, behavioral changes. | Moderate to Good (50-70% symptom reduction). | Emotional discomfort, time commitment. | Weekly sessions for several months to years. | High (learns coping skills). |
| Transcranial Magnetic Stimulation (TMS) | Uses magnetic fields to stimulate nerve cells in the brain. | Good (50-60% achieve remission for treatment-resistant depression). | Headaches, scalp discomfort. | Daily sessions for 4-6 weeks. | Moderate (booster sessions may be needed). |
Who Can Benefit? Ideal Candidates and Considerations
Neurofeedback for depression is a versatile treatment that can benefit a wide range of individuals. Ideal candidates often include:
- Individuals Seeking Non-Pharmacological Options: Those who prefer to avoid medication, or are looking for drug-free approaches due to side effects or personal philosophy.
- Those with Medication Intolerance or Insufficient Response: People who have tried antidepressants but experienced undesirable side effects or found them ineffective.
- Individuals Seeking Complementary Therapies: Neurofeedback can be an excellent adjunct to psychotherapy, medication, or other holistic approaches, potentially enhancing their effectiveness.
- Those with Co-occurring Conditions: Given its broad impact on brain regulation, neurofeedback can also help address co-occurring anxiety, ADHD, or sleep disorders often present with depression.
- People Committed to the Process: Neurofeedback requires consistent attendance and engagement. Individuals ready to commit to a series of sessions typically see the best results.
While neurofeedback is generally safe, it’s not a magic bullet. It requires patience and active participation. A thorough initial assessment with a qualified practitioner is essential to determine if neurofeedback is the right path for your specific situation and to set realistic expectations.
Potential Side Effects and Risks
Neurofeedback is widely considered a very safe procedure, especially when administered by a trained and certified professional. Unlike medication, it does not introduce foreign substances into the body, nor does it involve invasive procedures like surgery. Most reported side effects are mild, temporary, and often indicative that the brain is actively responding and adjusting to the training. These can include:
- Fatigue or Tiredness: The brain is working hard during a session, and some individuals may feel mentally tired afterward, similar to how one might feel after a strenuous workout.
- Mild Headaches: Infrequent and usually mild, often resolving quickly.
- Temporary Agitation or Irritability: As the brain begins to shift its patterns, some individuals might experience brief periods of heightened emotional sensitivity.
- Difficulty Sleeping: In rare cases, initial sessions might temporarily disrupt sleep patterns, though generally, neurofeedback tends to improve sleep over time.
These side effects are typically managed by adjusting the training protocols, duration of sessions, or frequency. It’s crucial to communicate any discomfort or unusual feelings to your practitioner immediately so they can fine-tune your personalized neurofeedback treatment. Serious adverse events are extremely rare, underscoring the overall safety profile of this brainwave training depression therapy.
Choosing a Neurofeedback Practitioner
The effectiveness of neurofeedback for depression largely depends on the skill and expertise of your practitioner. Selecting the right professional is a critical step. Here’s what to look for:
- Qualifications and Certification: Ensure the practitioner is certified by a reputable organization such as the Biofeedback Certification International Alliance (BCIA) or has equivalent advanced training in neurofeedback.
- Experience: Look for a practitioner with extensive experience specifically in using neurofeedback for depression and mood disorders.
- QEEG Expertise: A practitioner who utilizes QEEG brain mapping for initial assessment and ongoing monitoring demonstrates a commitment to evidence-based, personalized treatment.
- Holistic Approach: Ideally, they should understand how neurofeedback integrates with other mental health interventions and be willing to collaborate with your existing care team.
- Client Reviews and Testimonials: Look for positive feedback from previous clients, which can offer insights into their approach and success rates.
- Clear Communication: A good practitioner will clearly explain the process, set realistic expectations, and be transparent about costs and treatment duration.
Don’t hesitate to schedule an initial consultation to ask questions and gauge your comfort level with the practitioner. This is an investment in your mental health, and finding the right guide is paramount. Find a qualified neurofeedback specialist in your area.
Neurofeedback for Depression: Cost and Accessibility
Understanding the financial aspect of neurofeedback is important for prospective clients. The cost of neurofeedback for depression can vary significantly based on several factors:
- Location: Prices can differ between urban and rural areas, and across different regions or countries.
- Practitioner’s Experience and Qualifications: Highly experienced or specialized practitioners may charge more.
- Session Duration: Longer sessions might incur higher costs.
- Package Deals: Many clinics offer discounted rates for purchasing a series of sessions upfront.
- QEEG Mapping: The initial brain mapping often has a separate fee, ranging from a few hundred to over a thousand dollars.
On average, individual neurofeedback sessions can range from $100 to $250 per session. A full course of treatment (20-40 sessions) could therefore range from $2,000 to $10,000 or more. While this can seem like a significant investment, many view it as an investment in long-term mental health, potentially reducing the need for ongoing medication or therapy.
Insurance Coverage
Insurance coverage for neurofeedback for depression is evolving. While some insurance plans may cover it, particularly if it’s deemed medically necessary for conditions like ADHD or anxiety, coverage for depression can be less consistent. It’s crucial to contact your insurance provider directly to inquire about their policies regarding “EEG biofeedback” or “neurofeedback therapy” and to understand any requirements for pre-authorization or referrals. Some clinics may offer payment plans or financial assistance, so it’s always worth discussing options with your chosen provider. Learn more about navigating insurance for mental health services.
At-Home Neurofeedback Options
With advancements in technology, at-home neurofeedback depression devices are becoming more accessible. These systems typically involve a simplified EEG headset and software that guides you through training protocols. While they can be more cost-effective and convenient, they often lack the personalized QEEG assessment and expert supervision of a clinical setting. For serious conditions like depression, professional guidance is generally recommended, especially for initial assessment and protocol design. At-home systems might be best suited as supplementary tools or for maintenance after a course of clinical neurofeedback.
Integrating Neurofeedback into a Holistic Treatment Plan
For many, the most effective approach to managing and overcoming depression involves a holistic strategy that combines various therapeutic modalities. Neurofeedback for depression can play a powerful role within such a plan, working synergistically with other interventions to optimize mental wellness.
- Alongside Psychotherapy: Neurofeedback can make psychotherapy more effective by improving brain regulation. As the brain becomes calmer and more focused, individuals may find it easier to engage in cognitive behavioral therapy (CBT) or dialectical behavior therapy (DBT), process emotions, and integrate new coping strategies.
- Complementing Medication: For those who choose to use medication, neurofeedback can enhance its effects, potentially leading to greater symptom control or, under medical supervision, even a reduction in medication dosage. It helps the brain function more efficiently, reducing reliance on external chemical regulation.
- Lifestyle Adjustments: Combining neurofeedback with healthy lifestyle changes amplifies results. This includes a balanced diet rich in omega-3s and antioxidants, regular physical exercise, mindfulness practices, adequate sleep hygiene, and stress reduction techniques. These elements collectively support neuroplasticity and overall brain health.
- Nutritional Support: Addressing nutritional deficiencies with supplements like Vitamin D, B vitamins, and magnesium can further support brain function and mood regulation, creating a more fertile ground for neurofeedback to take effect.
By integrating neurofeedback into a comprehensive approach, individuals can create a robust framework for long-term mental health, moving beyond symptom management to genuine brain health optimization and sustained well-being. Discover holistic strategies for mental well-being.
Frequently Asked Questions About Neurofeedback for Depression
Q1: How quickly does neurofeedback work for depression?
A1: The timeline for experiencing results with neurofeedback varies greatly among individuals. Some people may notice subtle improvements in mood or sleep after just a few sessions, while others might require 10-15 sessions before significant changes become apparent. Generally, a full course of treatment (20-40 sessions) is recommended to achieve lasting and substantial improvements in symptoms of depression. Consistency in attendance is key to accelerating the process.
Q2: Is neurofeedback a permanent cure for depression?
A2: While neurofeedback can lead to significant and often long-lasting improvements in depressive symptoms, it’s more accurate to describe it as a powerful learning process that equips your brain with better self-regulation skills, rather than a “cure.” The brain learns to maintain healthier patterns, and for many, these changes are sustained for years. However, like any learned skill, occasional “booster” sessions might be beneficial for some individuals during times of high stress or if symptoms begin to re-emerge, ensuring the brain maintains its optimal state.
Q3: Are there any age restrictions for neurofeedback?
A3: Neurofeedback is generally considered safe and effective for a wide range of ages, from children (typically starting around age 5-6) to seniors. For children and adolescents, it can be particularly beneficial as their brains are highly plastic. For older adults, it can help maintain cognitive function and emotional resilience. The specific protocols and session structure may be adapted to suit the age and cognitive abilities of the individual.
Q4: Can I combine neurofeedback with antidepressant medication?
A4: Yes, neurofeedback can often be safely and effectively combined with antidepressant medication. Many individuals find that neurofeedback enhances the effects of their medication, potentially leading to greater symptom reduction or, under the guidance of their prescribing physician, even a gradual reduction in medication dosage over time. It’s crucial to inform both your neurofeedback practitioner and your prescribing doctor about all treatments you are undergoing.
Q5: What’s the difference between neurofeedback and biofeedback?
A5: Neurofeedback is a specialized form of biofeedback. Biofeedback is a broader term that refers to techniques used to gain control over involuntary bodily functions (like heart rate, muscle tension, skin temperature) using real-time feedback. Neurofeedback specifically focuses on regulating brainwave activity (EEG biofeedback). So, while all neurofeedback is biofeedback, not all biofeedback is neurofeedback.
Q6: Does insurance cover neurofeedback for depression?
A6: Insurance coverage for neurofeedback for depression varies. Some insurance plans may offer partial or full coverage, especially if it’s considered medically necessary and the practitioner is in-network. However, many plans still do not cover it or require specific diagnostic codes. It’s essential to contact your insurance provider directly to understand your benefits and potential out-of-pocket costs. Many clinics also offer superbills for out-of-network reimbursement or payment plans.
Q7: What does a typical neurofeedback session feel like?
A7: A typical neurofeedback session is generally relaxing and comfortable. You’ll sit in a comfortable chair, and sensors will be placed on your scalp (they only listen to brain activity, no electricity is sent in). You’ll then watch a screen or listen to sounds. The feedback is subtle – a video might play smoothly when your brain is in the desired state, or a sound might become clearer. It doesn’t involve pain or discomfort. Many people describe it as a calming experience, often feeling more relaxed and focused afterward.
Conclusion
Neurofeedback for depression stands out as a promising, evidence-based approach that empowers individuals to take an active role in their mental health journey. By directly addressing the brainwave dysregulation underlying depressive symptoms, this innovative brain training technique offers a path to more stable moods, improved cognitive function, and enhanced overall well-being. It’s a non-invasive, drug-free alternative or complement to traditional treatments, leveraging the brain’s remarkable capacity for change. If you’re seeking a sustainable and personalized solution to depression, exploring neurofeedback could be a transformative step towards reclaiming your mental vitality. Consult with a qualified neurofeedback specialist to discuss how this powerful therapy can be integrated into your personalized plan for lasting relief and resilience.








