Urinary Tract Infections (UTIs) are a common and often painful condition affecting millions worldwide. While uncomfortable, the good news is that UTIs are typically treatable with the right antibiotics. However, navigating the various options and understanding which antibiotic is best for your specific situation can be challenging. This comprehensive guide will delve into the world of UTI antibiotics, helping you understand their effectiveness, potential side effects, and crucial considerations for a successful recovery and long-term urinary health.
From identifying the symptoms to understanding antibiotic resistance and exploring preventive measures, we aim to equip you with the knowledge needed to make informed decisions about your health. Remember, while this article provides valuable information, it is not a substitute for professional medical advice. Always consult with a healthcare provider for diagnosis and treatment tailored to your individual needs.
Table of Contents
Understanding Urinary Tract Infections (UTIs)
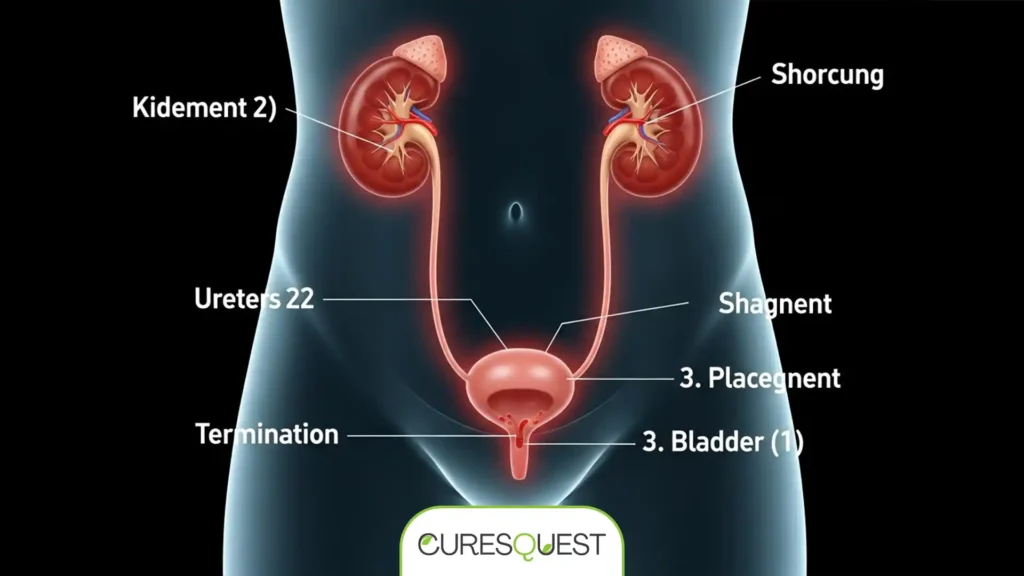
A UTI is an infection in any part of your urinary system — your kidneys, ureters, bladder, and urethra. Most infections involve the lower urinary tract, specifically the bladder (cystitis) and the urethra (urethritis). Women are more susceptible to UTIs than men, largely due to anatomical differences.
Common Symptoms of a UTI
Recognizing the symptoms early is key to prompt treatment. Common signs include:
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Passing frequent, small amounts of urine
- Cloudy urine
- Red, bright pink, or cola-colored urine (a sign of blood in the urine)
- Strong-smelling urine
- Pelvic pain in women — especially in the center of the pelvis and around the area of the pubic bone
If the infection spreads to the kidneys (pyelonephritis), symptoms can be more severe and include back pain, fever, chills, and nausea or vomiting. These cases require immediate medical attention.
How UTIs Are Diagnosed
Diagnosis typically involves a urine sample analysis. A urinalysis checks for white blood cells, red blood cells, and bacteria. A urine culture identifies the specific type of bacteria causing the infection and helps determine which antibiotics will be most effective. This is crucial for guiding the choice of the best antibiotics for UTI treatment.
The Best Antibiotics for UTI: A Detailed Overview
The choice of antibiotic depends on several factors, including the type of bacteria, the severity of the infection, patient allergies, and local resistance patterns. Here are some of the most commonly prescribed and effective antibiotics for UTI:
1. Trimethoprim-Sulfamethoxazole (Bactrim, Septra)
This combination antibiotic is a frequent first-line treatment for uncomplicated UTIs. It works by interfering with the bacteria’s ability to produce folic acid, which is essential for their growth. It’s generally well-tolerated but can cause side effects like nausea, vomiting, and skin rashes. Resistance to this drug has increased in some regions, so its effectiveness may vary.
2. Nitrofurantoin (Macrobid, Macrodantin)
Often prescribed for uncomplicated UTIs, especially in women, nitrofurantoin is effective because it concentrates in the urine and has minimal impact on beneficial gut bacteria. It’s a good choice for short-course treatment. Common side effects include nausea, headache, and gas. It’s generally avoided in patients with kidney problems.
3. Fosfomycin (Monurol)
Fosfomycin is unique as it’s typically given as a single-dose treatment. This makes it a convenient option for some patients, particularly those with uncomplicated UTIs. It works by inhibiting bacterial cell wall synthesis. Side effects are usually mild and can include diarrhea, headache, and nausea.
4. Cephalexin (Keflex)
A cephalosporin antibiotic, cephalexin is often used for UTIs, especially in pregnant women, as it is considered safe during pregnancy. It’s effective against a broad range of bacteria. Potential side effects include diarrhea, nausea, and abdominal pain.
5. Ciprofloxacin (Cipro) and Levofloxacin (Levaquin) – Fluoroquinolones
These are potent, broad-spectrum antibiotics often reserved for more complicated UTIs or when other first-line treatments are not suitable due to resistance or allergies. While highly effective, fluoroquinolones carry a black box warning from the FDA due to potential serious side effects, including tendon rupture, nerve damage, and psychiatric effects. They are generally not recommended as first-line treatment for uncomplicated UTIs unless absolutely necessary.

You can read more about the cautious use of antibiotics, including fluoroquinolones, by visiting the CDC’s guidelines on antibiotic use.
6. Amoxicillin/Clavulanate (Augmentin)
This combination antibiotic is sometimes used for UTIs, particularly when the bacteria are resistant to amoxicillin alone. The clavulanate helps protect amoxicillin from bacterial enzymes that would otherwise inactivate it. Side effects can include diarrhea, nausea, and yeast infections.
7. Doxycycline
While not a primary first-line treatment for uncomplicated UTIs, doxycycline may be used in specific cases, such as recurrent UTIs, or when other antibiotics are ineffective. It is a tetracycline antibiotic and can cause sun sensitivity and stomach upset.
Comparative Table of Common UTI Antibiotics
This table provides a quick reference for some of the best antibiotics for UTI, their typical uses, and important considerations.
| Antibiotic | Common Use | Key Considerations | Typical Dosage/Duration (Uncomplicated UTI) |
|---|---|---|---|
| Trimethoprim-Sulfamethoxazole (Bactrim) | First-line for uncomplicated UTIs | Growing resistance; potential for skin rash; avoid in sulfa allergy | 1 tablet twice daily for 3-5 days |
| Nitrofurantoin (Macrobid) | First-line for uncomplicated UTIs (especially women) | Concentrates in urine; less impact on gut flora; avoid in kidney impairment | 100 mg twice daily for 5-7 days |
| Fosfomycin (Monurol) | Uncomplicated UTIs; single-dose convenience | Single-dose therapy; generally well-tolerated | 3g sachet, single dose |
| Cephalexin (Keflex) | Uncomplicated UTIs; often used in pregnancy | Generally safe in pregnancy; good broad-spectrum coverage | 250-500 mg twice daily for 3-7 days |
| Ciprofloxacin (Cipro) / Levofloxacin (Levaquin) | Complicated UTIs; pyelonephritis; when resistance is present | Fluoroquinolone warnings (tendon rupture, nerve damage); generally not first-line for uncomplicated UTIs | 250-500 mg twice daily for 3-7 days (Cipro); 250-750 mg once daily for 3-5 days (Levaquin) |
| Amoxicillin/Clavulanate (Augmentin) | UTIs with specific resistance patterns; recurrent UTIs | Can cause GI upset and yeast infections | 500 mg/125 mg twice daily for 7 days |
Factors Influencing Antibiotic Choice
Choosing the right antibiotic is a nuanced process. Your doctor will consider:
- Type of Bacteria: Identified by a urine culture.
- Antibiotic Resistance: Bacteria can become resistant to certain antibiotics over time.
- Allergies: Known allergies to specific antibiotic classes.
- Medical History: Pre-existing conditions like kidney disease, diabetes, or pregnancy.
- Severity of Infection: Uncomplicated (bladder only) vs. complicated (kidneys, prostate, recurrent).
- Local Resistance Patterns: What antibiotics are most effective in your geographic area.
- Previous UTI Treatments: What has worked or failed in the past.
For more detailed information on managing urinary tract infections, consider exploring resources like this comprehensive urinary tract infection (UTI) guide.
Important Considerations During UTI Treatment
Proper antibiotic use is crucial for effective treatment and preventing antibiotic resistance.
Completing the Full Course of Antibiotics
Even if your symptoms improve quickly, it is vital to complete the entire course of antibiotics prescribed by your doctor. Stopping early can lead to a relapse of the infection and contribute to antibiotic resistance, making future infections harder to treat. This is a critical factor in ensuring the best antibiotics for UTI truly work.
Managing Side Effects
Antibiotics can cause side effects like nausea, diarrhea, or yeast infections. Discuss any concerns with your doctor. Probiotics may sometimes help mitigate gastrointestinal side effects, but consult your healthcare provider first.
When to Seek Further Medical Attention
If your symptoms worsen, don’t improve after a few days of antibiotics, or if you develop new symptoms like fever, chills, or severe back pain, contact your doctor immediately. These could indicate a more severe infection or a resistant strain of bacteria.
Preventing Recurrent UTIs
While antibiotics are effective for treating existing infections, prevention is key, especially for individuals prone to recurrent UTIs.

Lifestyle and Dietary Changes
- Stay Hydrated: Drinking plenty of water helps flush bacteria from your urinary tract.
- Urinate Frequently: Don’t hold urine for long periods.
- Wipe from Front to Back: This prevents bacteria from the anal region from spreading to the urethra.
- Urinate After Intercourse: Helps flush out any bacteria that may have entered the urethra.
- Avoid Irritants: Limit perfumed feminine products, douches, and spermicides, which can irritate the urethra.
- Cranberry Products: Some studies suggest cranberry products may help prevent UTIs, but evidence is mixed.
Medical Strategies for Recurrent UTIs
For individuals with frequent UTIs, your doctor might suggest:
- Low-Dose Antibiotics: A daily low dose for several months.
- Post-Coital Dosing: Taking a single antibiotic dose after sexual intercourse.
- Vaginal Estrogen: For postmenopausal women, to restore vaginal flora.
- D-Mannose Supplements: A type of sugar that may prevent bacteria from adhering to the urinary tract walls.
Understanding these preventive measures complements the use of the best antibiotics for UTI treatment, offering a holistic approach to managing urinary health. You can find more information on UTI prevention from reputable sources like the Mayo Clinic’s guide on UTI diagnosis and treatment.
Antibiotic Resistance and Future Challenges
One of the most pressing global health concerns is antibiotic resistance. Overuse and misuse of antibiotics contribute to bacteria evolving and becoming resistant, rendering traditional treatments ineffective. This phenomenon makes finding the best antibiotics for UTI increasingly challenging.
How Resistance Develops
Bacteria can develop resistance through various mechanisms, including genetic mutations or by acquiring resistance genes from other bacteria. When an antibiotic is used, it kills susceptible bacteria, but resistant ones survive and multiply, leading to a population dominated by resistant strains. This is why judicious use of antibiotics is paramount.
The Role of Healthcare Providers and Patients
Healthcare providers play a critical role by prescribing antibiotics only when necessary, choosing the narrowest spectrum drug possible, and ensuring appropriate dosages and durations. Patients must also do their part by taking antibiotics exactly as prescribed and not demanding antibiotics for viral infections (like colds or flu). The Harvard Health Publishing provides valuable insights into urinary tract infections and antibiotics, emphasizing responsible usage.
Special Populations: UTIs in Pregnancy, Men, and Children
UTIs in Pregnancy
UTIs during pregnancy require prompt and careful treatment, as untreated infections can lead to complications like preterm labor or kidney infections. Certain antibiotics, such as cephalexin and amoxicillin, are generally considered safe. Fluoroquinolones and tetracyclines are typically avoided. Regular screening for asymptomatic bacteriuria (bacteria in the urine without symptoms) is also common during pregnancy.
UTIs in Men
While less common, UTIs in men are often considered more complicated and warrant a thorough investigation to identify underlying causes, such as prostate issues or kidney stones. Treatment duration might be longer than for women, and specific antibiotics like fluoroquinolones or trimethoprim-sulfamethoxazole are frequently used. For further details on male UTIs, consulting resources like WebMD’s guide on antibiotics for UTIs can be helpful, though it focuses primarily on women, the principles of antibiotic action remain relevant.
UTIs in Children
UTIs in children can be challenging to diagnose due to non-specific symptoms. Prompt treatment is crucial to prevent kidney damage. Antibiotics like amoxicillin, cephalexin, or trimethoprim-sulfamethoxazole are commonly prescribed. Further evaluation for structural abnormalities in the urinary tract may be necessary for recurrent infections. The CDC offers guidance on antibiotic use for UTIs in the community setting, which includes considerations for various patient groups.
Emerging Treatments and Research
The fight against antibiotic resistance has spurred research into new treatment modalities. While still in early stages, some promising areas include:
- Vaccines: Development of vaccines to prevent recurrent UTIs.
- Bacteriophages: Viruses that specifically target and kill bacteria.
- Anti-Virulence Drugs: Medications that disarm bacteria by preventing them from causing disease, rather than killing them outright.
- Immunomodulators: Treatments that boost the body’s own immune response to fight infection.
These innovations offer hope for future strategies beyond conventional antibiotics, especially as resistance continues to rise. The NHS provides information on UTI treatments, including current and potential future approaches, highlighting the ongoing evolution in medical care.
Frequently Asked Questions
How quickly do antibiotics work for a UTI?
Most people start feeling relief from UTI symptoms within 24 to 48 hours after starting antibiotics. However, it’s crucial to complete the entire prescribed course to ensure the infection is fully eradicated and to prevent recurrence or antibiotic resistance.
Can I treat a UTI without antibiotics?
While mild UTI symptoms might sometimes resolve on their own, especially with increased fluid intake, antibiotics are generally necessary to effectively clear a bacterial infection and prevent it from spreading to the kidneys. Delaying antibiotic treatment can lead to more serious complications. Always consult a doctor for diagnosis.
What happens if I stop taking antibiotics early for a UTI?
Stopping antibiotics early can lead to several problems: the infection might return, it could become harder to treat (due to antibiotic resistance), or it could spread and become more severe, potentially affecting your kidneys.
Are there any natural remedies that help with UTIs?
Some natural remedies, like drinking plenty of water, cranberry juice (though evidence is mixed), and D-Mannose supplements, may help prevent UTIs or alleviate mild symptoms. However, they are not a substitute for antibiotics once an infection has taken hold. Always discuss natural remedies with your doctor.
How can I prevent recurrent UTIs?
Prevention strategies include drinking plenty of water, urinating after sex, wiping from front to back, avoiding irritating feminine products, and sometimes, for frequent sufferers, low-dose daily antibiotics or vaginal estrogen therapy (for postmenopausal women) as prescribed by a doctor.
Can men get UTIs, and are the treatments different?
Yes, men can get UTIs, though they are less common than in women. Male UTIs are often considered more complicated and may require longer courses of antibiotics and further investigation to identify underlying causes, such as prostate issues. The choice of antibiotics is similar but might be tailored to the specific cause.
What are the potential side effects of UTI antibiotics?
Common side effects include nausea, diarrhea, stomach upset, and yeast infections. More serious but rare side effects can occur, especially with certain classes like fluoroquinolones (e.g., tendon problems, nerve damage). Always discuss potential side effects with your doctor and report any unusual symptoms.
Conclusion
Urinary Tract Infections are a common ailment, and thankfully, effective antibiotic treatments are available. Understanding the best antibiotics for UTI, their proper usage, and the importance of completing your prescribed course is paramount for a successful recovery and preventing future complications. By working closely with your healthcare provider, staying informed about antibiotic resistance, and adopting preventive measures, you can effectively manage UTIs and maintain optimal urinary health. Remember, early diagnosis and appropriate treatment are key to alleviating discomfort and ensuring your well-being.







